DIEP Flap Reconstruction - the pretty(sic) way
On October 15, I got dressed for a pre-admit test at Houston Methodist. I’d taken the dreaded COVID test and with that underway, I could return to party mode. It was my 42nd birthday. My family and bestie had traveled from west and east to celebrate with me. But when the birthday dinner, game night, birthday brunch, and Tigerlily sponsored IG party were over, I was in reconstruction mode.
There were a few things that I needed to have done before I was admitted to the hospital. First, I had to tend to my daughter’s hair. It was time for a retightening of her locs, and five hours later I was free to pack my hospital bag. Since I knew that I would stay in the hospital between 3-5 days, I had a whole host of items in my overnight bag .. kindle, Bluetooth headphones, chargers, robes, toiletries, clothes to wear home among over things. Later I would realize that the ONLY item that I used in the bag was my phone charger. That’s all. In hindsight, I laugh at myself. Seriously, where did I think I was going? Sleepover camp? I didn’t even wear my retainer which I’ve worn every night for scores of years. Apparently, one cares little about straight teeth when you’re hospitalized. Go figure.
Fast-forward to the day before surgery. I’d scheduled an appointment with my therapist to get any low hanging drips of clarity before I went into surgery. I left there with a calm mind and reassurance that I was indeed ready for this next big step in my journey. At night I had an antibacterial shower and hours later when I awoke the next morning, I had another. No jewelry, No lotions, No perfumes or deodorants. Just me and my ridiculous hospital bag.
After a quick prayer with the family, Theo and I were off for the hospital. At 5 am, no one is on the road and we seemed to arrive in record time. The hospital is super dark and quiet at the hour. As I waited for Theo to adjust to the roof on the convertible, I was captured by the stillness of it all.
Pulled up with the Vote PSA
“Are you here for surgery?,” the woman behind the clear mask asked as I walked through the automatic doors. After information exchanged, I was given an armband (the first of many that would decorate my arm before I am admitted to the OR) and some patient id tags to give to surgery admittance. After 3 surgeries in 5 months, we were very familiar with the process. Theo signed as next of kin, and I was called back to change into attire for fitting for surgery, but not before another antibacterial wipe down. When he was ushered back, I was just as he’d seen me before .. with a purple robe and signature yellow hospital socks. I had to admit, the socks that I wore to the hospital that morning were much cooler if you asked me.
We are about one hour before my scheduled surgery time of 7:30. And this is when the visits from the multiple specialists begin. First, there is a nurse that asks the question that always tickles me. “Mrs. Parker, what are you here for today?” After we agree that I am the right person in the right place at the right time, I am rewarded with an IV in my arm. Next, the anesthesiologist appears to explain the procedure. It’s similar to the type of sedation that I’d had in prior surgeries except that this surgery (at 8 hrs) presented a greater risk for the need for a blood transfusion. I can’t say that I was excited about agreeing to this receive blood if needed, but what’s alternative ..bleeding out on the table? If I had known earlier, I may have asked to donate my own blown in the slight chance that I would need it during surgery.
Right on schedule, Dr. Shuck walked in just as bright-eyed and bushy-tailed as he could be. “You ready?”, h asked… “Yep, as ready as I will ever be!” Then he opened a fresh surgical marker and began drawing the framework for his newest masterpiece. With my husband by my side, I stood before Dr. Shuck almost as naked as I’d come into the world. There is something about the journey that I’ve gone through that makes me less apprehensive about showing my most private body parts. I never quite understood the vulnerability that my European colleagues spoke about when I lived in Belgium so many years ago. There, no one bats an eye at the sight of a breast. I think I’m finally there.
After he was satisfied, I pulled up my gown and like clock-work there was a knock at the door. And guess who it was LT, my breast surgeon. Although she wouldn’t be participating in today’s surgery, she popped in to wish me well and to participate in the photo ops. 🤣
They both head out and leave Theo and me alone with our thoughts. A chaplain enters the room to pray over the surgery and the hands that will perform God’s work. In an instant, he’s gone, the medical staff return and is ready to roll me out. And this is where the pre-anesthesia meds kick in for I don’t recall anything else after this point. The next thing I know, I am awake in the ICU - hot, cranky, and starving. I vaguely remember Theo standing over me whispering words that my brain will not allow me to recollect. I’m sure he said something like “you are the most beautiful post-surgery woman in the world, even with crud in the corner of your lips and chapped lips.” But just like that, he is gone.
On the large wall clock, I can see that it is nearly 8 pm. I count backward and calculate that I must have lost a few hours somewhere. This would mean that I had to be in surgery for at least 10 hours. Then I noticed that I am hot, and not just hot .. sweltering. As much as I can move my head, I look down at my body and make out the figure of what looks like a pool-float lying on top of me. There is hot air gushing out of it. It’s unbearable heat, like hot yoga. Later I would realize that the temperature measured 47 degrees Celsius .. more than 100 degrees F. Pure torture. A nurse comes in and explains that I need to keep my new breast warm because the greatest risk of FLAP death is within 24 hours of surgery. The heat keeps the blood flowing and there are also two boxes located at the end of the bed that display the hemoglobin and oxygen saturation levels in each breast. A lighted node was inserted into the lower portion of the DIEP flap so that the ICU nurse could use an ultrasound instrument (doppler pen) to monitor the flow each half-hour and then each hour. These measurements are automatically transmitted to my doctor’s phone. So he is aware of any risk of flap failure.
In the ICU, I go through a series of nurses with each shift change. But what remains consistent is their opinion of the result of my surgery. At each opening of my post-surgery bra to complete their routine, I notice a pause and then “Wow, they really look good.” Now, I couldn’t tell whether they were saying this for emotional support or not, but I’d heard it about 3x when the morning nurse walked in for her check. So I asked her to take some photos of my surgical sites. I wanted to see what they were seeing.
As an engineer, I have to admit that the technology was indeed cool but I wasn’t a fan of the constant prodding. It ensured that I got ZERO sleep the first night after surgery. Every hour someone was checking my incisions, my breasts, monitoring the blood flow, poking my finger to check my blood sugar (because the body does this weird thing when you have invasive surgery. A survival mechanism causes a spike in your blood sugar) and asking me to articulate my pain level. After this routine, I was rewarded with ice chips. When you haven’t consumed any food since 9 pm the night before, ice chips taste like strawberry shortcake with whipped cream on top. To pass the time between checks, I tried to ignore the gushing hot air by counting down the time until the leg wraps (which prevent blood clots) would inflate and send a light breeze of cool air up my legs. Every 90 seconds. That’s when I would receive my intermittent reward.
This went on until 7am the next morning, when the day nurse danced (literally) into my room waving a menu. Dr. Shuck had approved a diet. Thank God! I felt like I was at a 5 star restaurant in Paris. I ordered French toast, sausage, a hash-brown, grits, greek yogurt and cranberry juice. When my breakfast arrived, I had to eat in a weird position. Because I was not allowed to eat with my back perpendicular to my legs, I found myself in a pretty awkward position. Imagine a person lying one a beach chair with their knees slightly bent and their back elevated. That’s how I had to eat. (I know that this is the second reference that I’ve made to the beach .. with the beach float and now the beach chair, I am desperate need of a vacation, sorry) Well, as fabulous as breakfast was, I only managed to eat one French toast, a half of sausage and a piece of the hash brown. One of my surgeon’s PA’s had stopped by earlier to check on me. She warned that my stomach would feel even more tight after eating. She did not exaggerate. After only a few bites, it felt like a bowling ball was pushing through my abdomen. I wasn’t disappointed because I couldn’t eat another bite if I tried, but I did feel badly about wasting all of that food. I’d make a note for the next time it was time to order a meal.
Before I’d finished eating, my nurse was preparing for shift change. And just as she danced in with the menu, she sauntered in again with a special surprise - a cup of Starbucks. When placing my order, I noticed that there was coffee on the menu but I was hesitant to dabble. Overhearing my dilemma, we chatted about our Starbucks favs, and voila, moments later, she arrived bearing a gift - a venti skinny vanilla latte with nutmeg powder with a heart felt message on the lid.
Starbucks after surgery = heaven. In that same awkward position, I lay in the bed slowly sipping my latte out of a straw, when I notice a group of medical personnel wheeling a walker and a chair past the tall panel windows which give access to the hallway. “No, no, no, please don’t stop at my door. Please keep going. Please keep going. Shit!” They didn’t keep going. Two purple scrubbed PTs and two nurses enter my room. I looked at them in terror. “Good morning, Ms Parker. Do you know what time it is?” I look up, slightly annoyed .. Ummm, no. “It’s time to get out of the bed!” Crap! It’s not even 9am! They are talking amongst themselves and rearranging furniture and equipment in my room, but I don’t pay too much attention to them. I can’t take my eyes off of the chair that awaits me.
I’d not been in any pain since I arrived in the ICU, and I was very thankful for that. But I was certain that this would all change if I had to move from my bed to that chair. I just didn’t see how it could be feasible. Sitting up is what I did BEFORE surgery.. not 12 hours after the completion of my surgery.
Moving from a resting to a sitting position was only half the battle. Once I managed to move one leg at a time and roll myself up to the edge of the bed, that’s when the trust came in.
Sitting up on my own
I had to trust myself, my legs and my abs, and I had to trust those PTs that had been moving patients for years..
And on Day 2 at 9 am, I did it. I moved from the bed to the chair. And still, incredibly, I had no pain. I was relieved, elated, and more than that, I was empowered. If I could move from the bed to the chair with no pain.. what else could I do?
From the bed to the chair.. A huge accomplishment
They’d removed my catheter before I moved to the chair. So my butt would not be a permanent fixture in the chair. Within the day, I’d get up from that chair twice to use the toilet that was hidden under a small sink behind my chair. I didn’t even know it was there until one of the cleaners flushed the toilet as I was sitting there.
I was so amazed that I did not need pain medicine. More like confused. “Maybe it’s adrenaline,” I thought. I’d had a major invasive surgery after all. At some point, I became obsessed. I needed to know more about the pain management system that Dr. Shuck elected to use for my procedure. Before leaving, the nurse connected my phone to Alexa so that I could listen to music, but this research project felt like a more fulfilling way to past the time. I slightly recalled the acronym ERAS, and I went to google for some clarity.
ENHANCED RECOVERY AFTER SURGERY (ERAS) is a multimodal perioperative care pathway designed to achieve early recovery for patients undergoing major surgery. It represents a paradigm shift in perioperative care in two ways. First, it eliminates opioid use. (The opioid crisis, in which addiction and harm are related to pain-relieving opioid drugs, has been well documented in the US) Second, it is comprehensive in its scope, covering all areas of the patient’s journey through the surgical journey.
ERAS allow patients to recover much faster after their operation and this reduces the need for hospital stay by about 30% or more than 2 days after major abdominal surgery.
The key factors that keep patients in the hospital after surgery include the need for parenteral analgesia, the need for intravenous fluids secondary to gut dysfunction, bed rest caused by lack of mobility. And this is why I was out of the bed at 9am on Day 2!
Before surgery, Dr. Shuck told me that he would be utilizing a pain management technique that would avoid use of narcotics. I was ecstatic. I don’t like to take medicine, especially narcotics. But I wondered how it would be possible to manage post surgery pain with Tylenol? The magic starts with the injection of a cocktail of extended release lidocaine medicine all over the surgical sites in the OR. After which, I was on a regimen of scheduled Tylenol for pain, Celebrex (anti-inflammatory), Neparin (nerve pain), and a mild muscle reliever. No narcotics. Of course, there were stronger pain relievers available should I request it, but I never had the need to. I only experienced slight pressure in my abdominal area which is to be expected after the “snatch” that I received. 🤣
When you have your consult with your surgeon to discuss the process and recovery time for your breast reconstruction, ask the question, “Do you use the ERAS protocol at the facility I will be having my surgery?” In my opinion, it’s worth the ask!
Satisfied with what I’d found on the internet, I began to enjoy the second stage of my Starbucks coffee.. (the lukewarm experience). That’s when a tall, dark haired gentlemen stopped outside my door, reached for anti-bacterial hand cleaner and walked in. I’d seen him before but I could not place him until he started speaking. It was Dr. Echo, the other plastic surgeon who supported Dr. Shuck during my surgery. (Generally, DIEP Flap (micro-surgery) is a long surgery which requires more than one doctor at the OR table.) He confirmed that there were no complications during my surgery. Everything had gone smoothly. My breasts were pretty symmetric, even after the removal of the necrotic skin on the right breast.
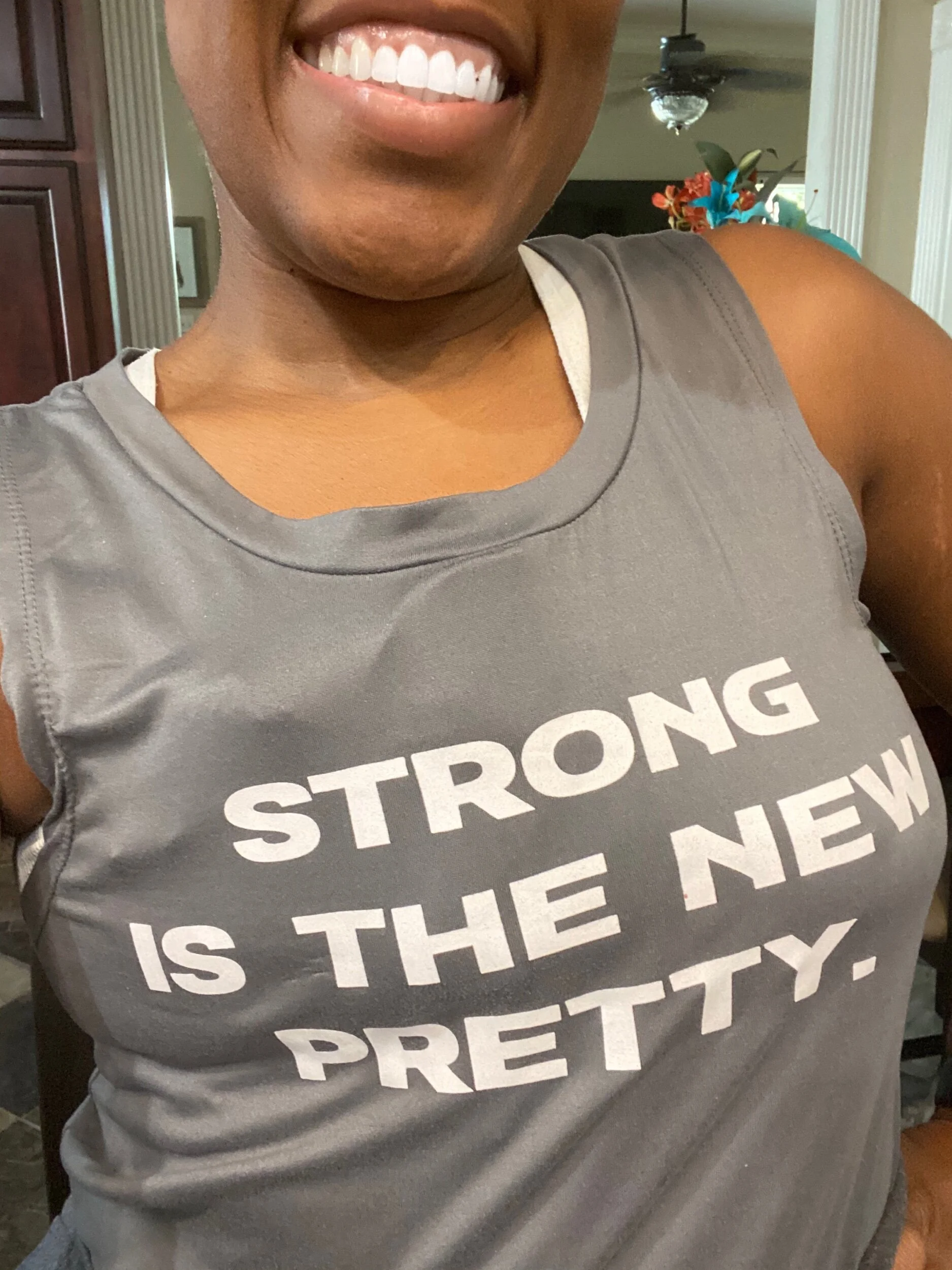
But then, he said something that made me grin from ear to ear.. Ok, I know, I always grin from ear to ear but even more so this time. He said, and I quote “Your muscles were ripped under that tissue that we removed. What are you doing cross-fit every day?” OMGeeeee, you would have thought he told me that I won a million dollars. So apparently, under these extra 25 pounds, those muscles are patiently waiting for their time. This was a gift and a curse, on one hand they didn’t have to do any muscle tightening for aesthetics but on the other hand I’d likely feel more pressure when doing normal activities like eating, coughing, laughing, etc.. Check, check, and check .. been there and done that Doc.
He warned me to take it easy in the meantime. Remember to hunch over when walking to avoid damaging my stomach incision. No exercise for about 6 weeks.. This works well with my plan as the rebuild of Tova 2.0 starts in 2021.
Lastly, I learned that I would be moving out of the ICU that day and home on Friday. Dr. Echo had dropped little pockets of sunshine in my room before he left. Soon after, Theo had arrived and we compared notes. I’d had one too many coughing fits brought on from the irritation of the breathing tube. Let’s see how I can explain trying to cough after a DIEP Flap procedure. Well, you feel the cough in your chest but you try to reduce one big cough into multiple baby coughs because your stomach can absorb the pressure of multiple small coughs. But at some point you have to put your big girl panties on and toughen up for one big cough so the fit can be over. This can last any where from seconds to a minute. But it seems like forever!!! You can’t talk and you’re gasping for air while holding a pillow across your belly..
Theo suggested that I request a popsicle. Well, the popsicle didn’t stop the cough. But it definitely made my throat feel better. I don’t know how many of these I’d eaten before I was wheeled from my room in the ICU to a normal recovery room in a recliner chair no less. They were really serious about only being in the bed when you were sleeping.
probably ate a whole box of these things …
Being out of the ICU meant that I wouldn’t be checked every hour. I was officially out of the danger zone, though some small risk still existed. The same checks would be done but I would only be monitored every 4 hours instead of every hour. Translation: More SLEEP! As an additional bonus, visiting hours would also be extended.
The first thing that I did when I was introduced to my my nurse was ensure that she understood the care that I required. The medicine schedule, the heat required to ensure blood circulation, the doppler ultrasound .. I needed to know that she understood it all. Sure, the nurses have discussions during custody transfer, but it is up to me to advocate for my care. Lucky for me, my nurse, Sophie, was very familiar with my needs. Her family member had been recently diagnosed with breast cancer and she had the same procedure and was treated by my secondary doctor, Dr. Echo. Look how God works! 🙌🏾 I was in good hands!
photo: me and Sophie
Me and sweet Sophie
That night, I was at ease. I was sure that the transition of my care would be seamless with Sophie by my side. I slept like a baby. At 6 am, Sophie and her peer walked in and turned on the bright overhead light in my room. “Good morning Mrs Parker. It’s time to get up.” 6AM.. Really? I couldn’t believe it was time to get up. The last I remembered I’d just gotten in the bed after dinner. I had not remembered the scheduled meds that she’d given me in the middle of the night or the gentle probing of my breasts to check for blood flow. I’d officially had a good night’s sleep.
On the morning of day three, and after two nights in the hospital, I wanted a shower .. desperately. Unfortunately, Dr. Shuck delayed my request when he arrived that morning to check me out. But just like Dr. Echo, he left only after leaving buckets of sunshine. After checking my incision and breasts, he confirmed that I was out of the danger zone. Since I’d been drinking water and urinating regularly, he told the nurse to remove my IV. He told me that I needed to walk 3 times that day, I could shower the following day and that I could also go home the following day. 🎉 Suddenly, I didn’t care about the shower anymore.
I ordered a much lighter breakfast this time. I’d learned that I wasn’t able to put down as much food as I had in the past. By the time I’d finished eating, Theo had arrived. The goal for the morning was to eat, use the restroom, and then take my first walk. My nurse guided me and around the floor. Prepared for wither a fall or fatigue, she braced for a fall with a left hand and rolled a chair in her right hand. I made it around the floor and then I needed a break. I wasn’t light headed or dizzy but my back hurt from walking hunched over. I couldn’t wait to get back to my chair. Once I was there, it was time for my scheduled muscle relaxer. Right on time. I felt a nap coming on, so I sent Theo home to finish working. He could return in the evening for a short visit. There was no need for him to watch me sleep.
No sooner had he left and I been comfortably placed back in my chair had the PT team come to take me for a “walk.” Surely they had to be kidding. I’d just walked 1o minutes before. But as I understood it, they needed to document an ambulatory report in order for me to be discharged. Once each day. That was all I needed to hear. Just like that, I was up and walking. They were satisfied that I didn’t need a walker and they told me that it counted as walk #2 for the day.. Works for me - 2 down, 1 to go.
Once I’d gotten back to my chair, I awoke to a personal pizza which was far too large for me to consume. My nurse suggested eating a slice once an hour until dinner. She reminded me that proper diet is required for healing. I’d been sleeping on and off since 2 pm, so each time I awoke, I ate a slice of the pizza. The last time I awoke it was 6pm and Theo’s voice startled me as it echoed behind my chair. He’d been there since 5pm, just after I’d finished off my pizza.
Took me 4 hours to eat this little thing
Just like that, it was time to order dinner .. again. The plan was to order dinner, use the restroom again, take my last walk, and then transfer from move directly to the bed. With later hours on this recovery floor, Theo hung out with me for a while. As I inched back and forth past the door, I heard him yelling “Go Speedy.” 🤣 As I pushed myself to reach the far end of the hall, Mary (the PT who had helped me out of bed the day before) jumped in front of me. Together we did a little “Discharge” dance, and a few moments later I back in my room. Theo had gone and my body was relaxing after a low-dose valium. I decided tp FaceTime my cousin, Shonta before I fell asleep.
A few minutes into our conversation, I had one of my famous coughing fits. But this one was a major one. I tried desperately to convert that big cough into baby coughs, but it just wasn’t working. My stomach rumbled like thunder with each cough. I dropped my phone and reached for the call button. The nurse who answered asked if I was throwing up, but I could only respond to here in quick baby coughs. She couldn’t understand me. Shonta could know longer see me because the phone was now facing the ceiling, and I couldn’t stop coughing. At some point the phone disconnected and the nurse appeared with a vomit bag. Once he realized that I only needed tolerate my position, the coughing fit was done. Problem solved.
I called Shonta back and she was on the other line with someone at the hospital. When the phone disconnected, she could not tell if aI got the care I needed so she took matters into her own hands. While this is the most endearing, caring, and sweetest thing that someone could do in this situation, I only remember her face when she answered the call the second time. And I just started laughing which caused another coughing fit. For some reason, she didn’t find the humor in it..
When I awoke the next morning on Day 4, my eyes were glued to the door. It was discharge day! I couldn’t wait for Dr. Shuck to stop by. I wasn’t really hungry but I figured it would pass the time so I ordered something light with protein. Oatmeal and yogurt. Just as I was finishing up, Dr. Shuck came in. He unhooked the lightbulbs from my breasts and turned off the monitors. He talked about medicine that I would take at home and the fact that I hadn’t taken any narcotics after major surgery. He really thinks that ERAS is the future of pain management. I would have to take all 6 drains home and continue to walk with a slight hunch. I asked him about my elevated glucose levels. He agreed that it was natural for glucose levels to spike after major surgery. But with weight loss, my levels would return to normal. Often, some people transition from one major health trial to another because they fail to manage the symptoms that they collected along the way.
Once the news was out that I was being discharged, all types of people came to visit.
My nurse brought my bag of goodies for home: washcloths, antibacterial soap, bras, wipes. And a stack of reading material.
The nurse navigator inquired about my home environment. She wanted to ensure that I had adequate care at home that would willingly support my recovery. She also wanted to be sure that I didn’t feel threatened at home and that I was not a victim of abuse.
The physical therapists team stopped by for a final walk. They asked me what I was told to do at home. We walked all the way to the other end of the hall. No cane, no dizziness, no support just me and my baby steps. Half way up the hall, someone jumped in front of me. It was Mary the PT who had helped me out of bed on day 2. We did a little dance to celebrate my discharge. I tapped the wall at the end of the hall, and turned around again. Success! I’d made it back to the chair.
Finally, the rep from case mgmt stopped by to tell me that by law I did not have to leave if I felt it was too soon. I had 4 hours to appeal the discharge and gave me the number to call. In the meantime, she told me that she prayed for me this morning and will do so again this evening. “You’re on my list butterfly.” Such a perfect name as I planned to flutter out of there.
Once Dr. Shuck submitted the required documentation, my nurse told me to have my ride there in 45 minutes. I was really going home. Just before I left, the charge nurse came in to check on my stay. I told her that I would rate them an 11 on a scale of 1-10 if I could. She asked me about my journey and shared some information about her concern with mammograms. I told her to trust her intuition. If she feels something, then force them to listen to her. She has to advocate for herself. There is and will never be a better advocate.
At 2pm, I was being wheeled to the front of the hospital. I waved goodbye to the awesome team of nurses and told them that I hope I’d never see them ever again. As the elevator door closed, I noticed a word on the wall that perfectly summed up my experience.
Thanks to Houston Methodist Willowbrook for taking care of me during my stay.